In our previous posts (June 2017 and October 2017) we explained two of our studies looking at the role of truncating variants in the Titin gene (TTNtv) in dilated cardiomyopathy (DCM). In the first of these, we found that having a TTNtv meant that a DCM patient was more likely to have had a past history of abnormal heart rhythms when they were first diagnosed with DCM. But we did not have enough data to definitively assess whether this was due to rhythms in the upper (atrial) chamber of the heart, the bottom (ventricular) chamber, or both. We also didn’t know whether this meant that DCM patients with a TTNtv were at higher long-term risk of potentially dangerous or life-threatening heart rhythm abnormalities. In our second study, we followed up a large group of patients with DCM but didn’t find an increased rate of major arrhythmic events in patients with a TTNtv. As a whole this group had relatively mild symptoms of DCM at the time of the study (the majority being in NHYA class I/II heart failure), with moderately impaired ventricular function – which puts them in a comparatively low-risk group for arrhythmias. Perhaps as a result, the overall rate of arrhythmic events in the study was low, making it harder to see subtle differences between those with and without a TTNtv.
To investigate further, we therefore started a new study on patients with DCM who also had an implantable cardiac device (ICD or CRTD). Not only are patients with these devices more likely to have an arrhythmia (they are typically given to the patients because they have worse heart function or symptoms) but, crucially, they monitor the patient’s heart rhythm 24-hours a day, 7-days a week. This allowed us to get complete coverage of each patient’s heart rhythm data over a number of years.
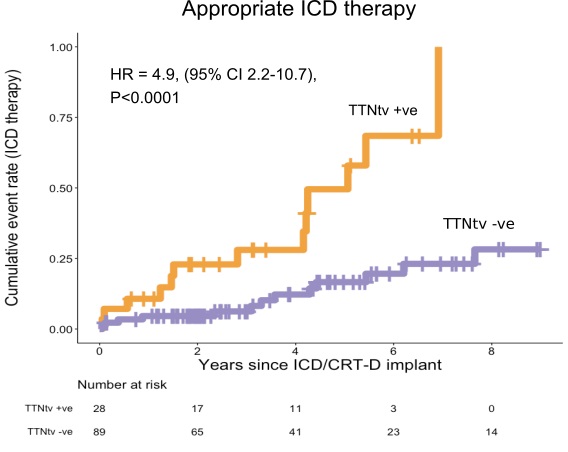
Our study, which was published earlier this month in JAMA: Network Open, found that TTNtv are associated with a significantly higher risk of both ventricular and atrial arrhythmia in DCM patients with an ICD or CRTD.
We had a strict definition of arrhythmia, for example only counting a ventricular arrhythmia if it was both fast (>200 beats per minute) and prolonged. These are the rhythms considered to pose the most danger to patients.
Importantly, we looked at the other major factors known to increase the risk of arrhythmia – age, male sex, level of left heart dysfunction and presence of heart fibrosis (scarring) on MRI – and even after controlling for these statistically TTNtvs were a strong predictor of arrhythmia.
Heart fibrosis, or scarring, on MRI is worth delving into a little more deeply. Fibrosis shows up as white patches on the heart in an MRI scan after a contrast agent (gadolinium) has been given via a vein. The presence of this fibrosis has long been known to be a strong predictor of arrhythmia, it’s likely that the scarred area interferes with the way electrical signals travel through the heart. DCM patients with a TTNtv don’t seem to have more fibrosis than other DCM patients – we found that in a previous study and confirmed it again here. However, a remarkable finding in our study was the apparent additive nature between fibrosis and a TTNtv in terms of arrhythmia risk. Of those patients that had both fibrosis and
a TTNtv, 62% experienced a ventricular arrhythmia, compared to only 5% of those with neither fibrosis or a TTNTv.
So how might TTNtvs lead to more arrhythmia in DCM?
This study wasn’t designed to answer this question and much more work needs to be done. But one avenue worth investigating is the fact that DCM patients with a TTNtv seem to have thinner heart muscle walls than those without a TTNtv, as we discussed in one of our previous blogs from October 2017. Thinner walls lead to increased ‘strain’ on the heart muscle cells, which can potentially alter their electrical properties.
Can knowing if a patient has a TTNtv help decide whether or not they should have an ICD? This was a relatively small study and the robustness of the findings certainly needs to be tested in much larger cohorts. Such studies are under way (see our blog post from October 25th 2018) and it is hoped that in the future TTNtv may be one of several factors that can help in risk-stratifying patients with DCM.
You can read our published study here: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2736938
Post by Ben Corden