Researchers from the Cardiovascular Genetics & Genomics Group have published their latest findings in Open Heart journal, using the Heart Hive platform to connect with people with cardiomyopathy. The paper assesses the effects of the first wave of COVID-19 pandemic on patients with cardiomyopathy using three parallel approaches.
The study has demonstrated that a third of the surveyed patients with cardiomyopathy felt that their physical health deteriorated as a result of the pandemic when assessed shortly after the first wave of the pandemic. This was a significantly higher proportion than those that had reported a suspected COVID-19 infection.
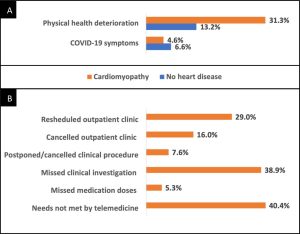
The study further illustrated that many patients had had outpatient clinic appointments rescheduled (29%) or cancelled (16%), and missed clinical investigations (38.9%), procedures (7.6%) or doses of medication (5.3%). Additionally, 40.4% of patients with cardiomyopathy felt that their health needs could not be met by telemedicine.
The findings also indicated that the psychological impact of the pandemic did not differ significantly between patients with cardiomyopathy and subjects without heart disease. Patients with cardiomyopathy did feel that they may be more susceptible to COVID-19 infection and suffer more severe illness if infected.
Approximately 1 in 5 patients with cardiomyopathy had received a recommendation to ‘shield’; a higher proportion of the patients that had received a recommendation to shield reported worsening of their cardiomyopathy symptoms.
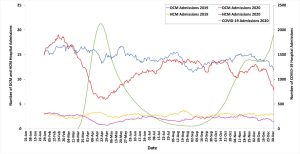
We also conducted two other parallel research initiatives alongside the Heart Hive COVID-19 study, which are also published in this article. By studying participants of the Royal Brompton & Harefield Hospital Cardiovascular Research Centre Biobank, we found that patients with DCM and HCM were no more likely to be infected with COVID-19 than the rest of the UK population. However, of the patients with DCM and HCM that were studied, those that had been infected with COVID-19 had more frequently required treatment in hospital during the first wave of the pandemic.
Finally, we used NHS Digital Hospital Episodes Statistics to illustrate that there was a 17.9% year on year reduction in cardiomyopathy-related hospital admissions in 2020, with the lowest hospitalisation rate occurring during the first UK lockdown.
To the best of our knowledge, this is the first study to assess both the direct and indirect effects of the COVID-19 pandemic on patients with cardiomyopathy. We hope these findings can be used to adapt clinical services to meet patients’ health needs as the pandemic evolves.
We are very grateful to the Heart Hive participants who contributed to this research initiative and to Cardiomyopathy UK for their ongoing support of this study and the Heart Hive. If you’re taking part in the study, please keep completing your COVID surveys to help us see how COVID-19s effect on people with cardiomyopathy has been changing during the course of the pandemic and with the developments of vaccines and new treatments.
If you haven’t signed up the the Heart Hive and would like to, you can find out more on the Heart Hive home page.